A Review Article: Fall Incidents and Interior Architecture— Influence of Executive Function in Normal Ageing
Main Article Content
Abstract
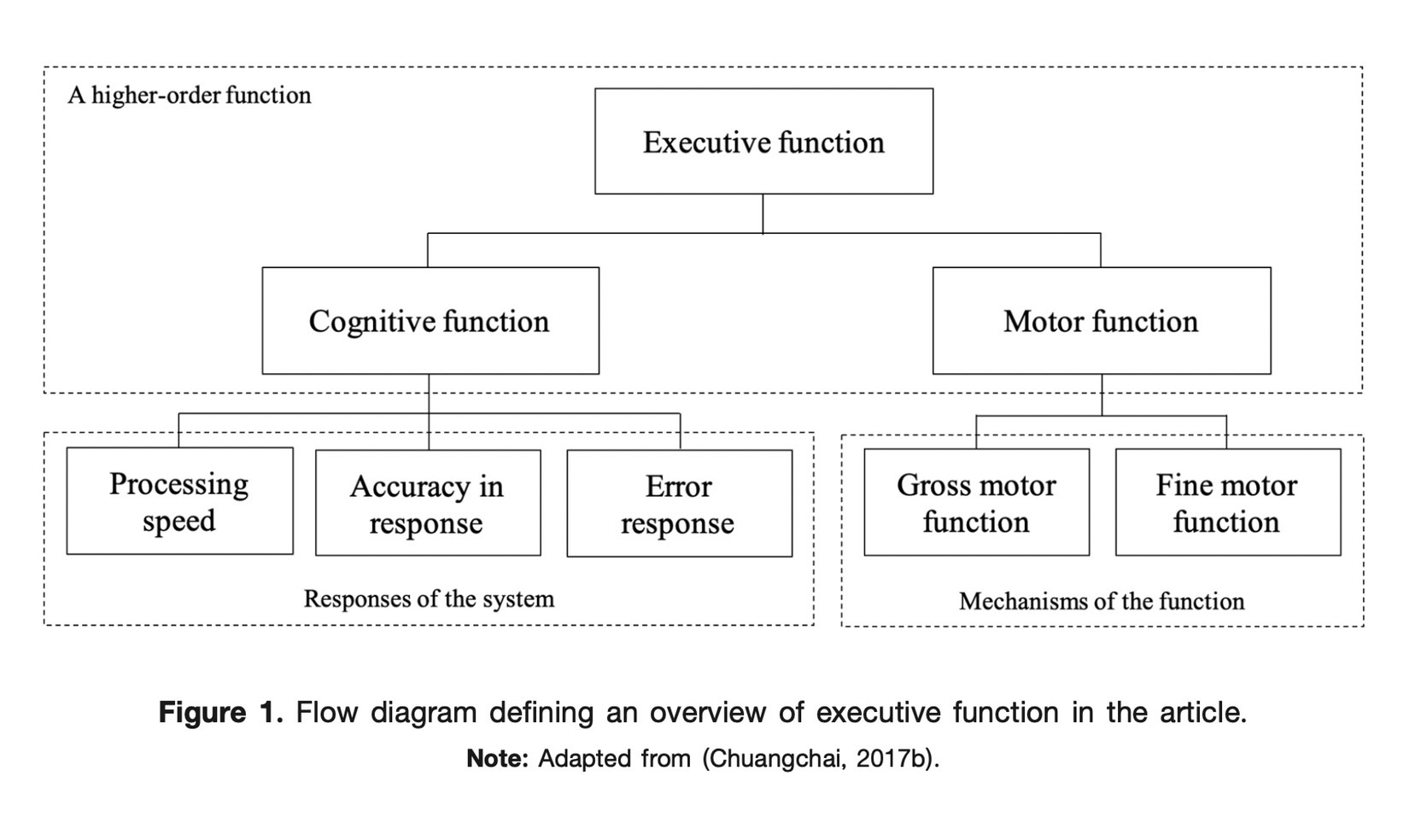
Many ageing people are staying at home, whether they are self-isolating or social distancing, because of the current Covid-19 situation. Fall incidents at home among the ageing are significantly associated with a high level of mortality. Bathrooms are frequently reported as a major environmental hazard in connection with falls. This serious health risk raises the matter of interior architecture. In terms of preventing falls, more architectural research focuses on interior elements e.g., handrail design, and non-slip mat, whilst less attention is paid to the issue of how ageing causes falls. Therefore, this article sheds light on the normal ageing process through an executive function that helps in the fall prevention of ageing people via decision-making and problem-solving. Normal ageing gradually results in declining executive function, including cognitive and motor functions, which limits and reduces day to day activities. The cognitive function (as a system) involves processing speed, accuracy in response, and error response whereas the motor function (as a mechanism) defines both gross and fine motor functions. A combination of cognitive and motor functions reflects conditions that may lead to a fall. Regarding the executive function, interior architecture for preventing falls in normal ageing people is strongly encouraged e.g., clear layout, timesaving activity, simplicity of design, lighting uniformity, short walking distance, cased opening, lightweight fixtures, and fine texture flooring. This article reviews the literature to address the knowledge gaps between interior architecture and human-centred design through ageing ergonomics, and employs a behaviour-focused aspect to interpret results for interior architects. Electronic databases, including Scopus, PubMed, and Google Scholar, were searched to specify appropriate papers, which were restricted to those in the English language. To improve the quality of the elderly’s life, this article provides recommendations that could assist interior architects in this challenge.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
All material is licensed under the terms of the Creative Commons Attribution 4.0 International (CC-BY-NC-ND 4.0) License, unless otherwise stated. As such, authors are free to share, copy, and redistribute the material in any medium or format. The authors must give appropriate credit, provide a link to the license, and indicate if changes were made. The authors may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use. The authors may not use the material for commercial purposes. If the authors remix, transform, or build upon the material, they may not distribute the modified material, unless permission is obtained from JARS. Final, accepted versions of the paper may be posted on third party repositories, provided appropriate acknowledgement to the original source is clearly noted.
References
Ahasan, R., Campbell, D., Salmoni, A., & Lewko, J. (2001). Ergonomics of living environment for the people with special needs. Journal of Physiological Anthropology and Applied Human Science, 20(3), 175–185. https://doi.org/10.2114/jpa.20.175
Ball, K., Edwards, J. D., & Ross, L. A. (2007). The impact of speed of processing training on cognitive and everyday functions. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 62 Spec No 1, 19–31. https://doi.org/10.1093/geronb/62.special_issue_1.19
Ballesteros, S., & Mayas, J. (2015). Selective attention affects conceptual object priming and recognition: A study with young and older adults. Frontiers in Psychology, 5, 1567. https://doi.org/10.3389/fpsyg.2014.01567
Berryman, N., Bherer, L., Nadeau, S., Lauzière, S., Lehr, L., Bobeuf, F., Lussier, M., Kergoat, M. J., Vu, T. T., & Bosquet, L. (2014). Multiple roads lead to Rome: Combined high-intensity aerobic and strength training vs. gross motor activities leads to equivalent improvement in executive functions in a cohort of healthy older adults. Age (Dordrecht, Netherlands), 36(5), 9710. https://doi.org/10.1007/s11357-014-9710-8
Brébion G. (2001). Language processing, slowing, and speed/accuracy trade-off in the elderly. Experimental Aging Research, 27(2), 137–150. https://doi.org/10.1080/036107301750073999
Buchman, A. S., Boyle, P. A., Wilson, R. S., Fleischman, D. A., Leurgans, S., & Bennett, D. A. (2009). Association between late-life social activity and motor decline in older adults. Archives of Internal Medicine, 169(12), 1139–1146. https://doi.org/10.1001/archinternmed.2009.135
Camicioli, R., Moore, M. M., Sexton, G., Howieson, D. B., & Kaye, J. A. (1999). Age-related brain changes associated with motor function in healthy older people. Journal of the American Geriatrics Society, 47(3), 330–334. https://doi.org/10.1111/j.1532-5415.1999.tb02997.x
Cammen, T. J. M. v. d., Wang, G., & Albayrak, A. (2019). Where ergonomics meets geriatrics: the connection between comprehensive geriatric assessment and design for ageing. European Geriatric Medicine, 10(3), 333–335. https://doi.org/10.1007/s41999-019-00171-7
Chiu, H. L., Chan, P. T., Kao, C. C., Chu, H., Chang, P. C., Hsiao, S. S., Liu, D., Chang, W. C., & Chou, K. R. (2018). Effectiveness of executive function training on mental set shifting, working memory and inhibition in healthy older adults: A double-blind randomized controlled trials. Journal of Advanced Nursing, 74(5), 1099–1113. https://doi.org/10.1111/jan.13519
Chuangchai, W. (2017a). Association among fear of falling, stress, and quality of life in adults and older people. Journal of Architectural/Planning Research and Studies (JARS), 14(2), 31-40.
Chuangchai, W. (2017b). Effect of Cognitive Plasticity Training on Falling in Aging. [Doctoral dissertation, Thammasat University]. Thammasat University. https://ethesisarchive.library.tu.ac.th/thesis/2017/TU_2017_5710300335_6844_9239.pdf
Chuangchai, W. (2017c). A review article: Environmental hazards at home and ergonomics as fall prevention for elderly population. Journal of Architectural/Planning Research and Studies (JARS), 14(1), 1-20.
Chuangchai, W. (2020). Pulse transit time in ageing as early biomarker for risk of dementia. Thai Journal of Ergonomics, 3(1), 35-44.
Chuangchai, W., & Pothisiri, W. (2021). Postural changes on heart rate variability among older population: A preliminary study. Current Gerontology and Geriatrics Research, 2021, 6611479. https://doi.org/10.1155/2021/6611479
Chuangchai, W., Pothisiri, W., & Chanbenjapipu, P. (2021). Variation of autonomic nervous system function by age and gender in Thai ischemic stroke patients. Brain Sciences, 11(3), 380. https://www.mdpi.com/2076-3425/11/3/380
Chuangchai, W., & Siripakarn, Y. (2017). Effect of cognitive and motor plasticity training on aging between non-fallers and fallers [Paper presentation]. The 2017 WEI International Academic Conference Proceedings, Harvard University, Boston, USA.
Chuangchai, W., & Siripakarn, Y. (2018a). Combined training’s effects on elderly people’s development to minimize risk of falling. West East Journal of Social Sciences, 7(1), 1-12.
Chuangchai, W., & Siripakarn, Y. (2018b). Falling and aging: Impact of cognitive and motor plasticity training. The Journal of Aging and Social Change, 8(3), 27-36. https://doi.org/10.18848/2576-5310/CGP/v08i03/27-36
Chuangchai, W., & Siripakarn, Y. (2019). Executive function training in connection with falls on elderly Thais. Journal of Population Ageing, 12(2), 137-149. https://doi.org/10.1007/s12062-019-9239-9
Chuangchai, W., & Suwanprasert, K. (2015). Guidelines to developing design for sustainability for senior citizens in Thai society [Paper presentation]. The 4th International Symposium on Engineering, Energy and Environments, Thammasat University, Pattaya Campus, Chonburi, Thailand.
Curreri, C., Trevisan, C., Carrer, P., Facchini, S., Giantin, V., Maggi, S., Noale, M., De Rui, M., Perissinotto, E., Zambon, S., Crepaldi, G., Manzato, E., & Sergi, G. (2018). Difficulties with fine motor skills and cognitive impairment in an elderly population: The Progetto Veneto Anziani. Journal of the American Geriatrics Society, 66(2), 350–356. https://doi.org/10.1111/jgs.15209
Ebaid, D., Crewther, S. G., MacCalman, K., Brown, A., & Crewther, D. P. (2017). Cognitive processing speed across the lifespan: Beyond the influence of motor speed. Frontiers in Aging Neuroscience, 9, 62. https://doi.org/10.3389/fnagi.2017.00062
Eckert, M. A., Keren, N. I., Roberts, D. R., Calhoun, V. D., & Harris, K. C. (2010). Age-related changes in processing speed: Unique contributions of cerebellar and prefrontal cortex. Frontiers in Human Neuroscience, 4, 10. https://doi.org/10.3389/neuro.09.010.2010
Ferguson, H. J., Brunsdon, V. E. A., & Bradford, E. E. F. (2021). The developmental trajectories of executive function from adolescence to old age. Scientific Reports, 11(1), 1382. https://doi.org/10.1038/s41598-020-80866-1
Fisher, G. G., Chacon, M., & Chaffee, D. S. (2019). Chapter 2 - Theories of cognitive aging and work. In Boris B. Baltes, C. W. Rudolph, & H. Zacher (Eds.), Work Across the Lifespan (pp. 17-45). Academic Press.
Fjell, A. M., Sneve, M. H., Grydeland, H., Storsve, A. B., & Walhovd, K. B. (2016). The disconnected brain and executive function decline in aging. Cerebral Cortex, 27(3), 2303-2317. https://doi.org/10.1093/cercor/bhw082
García-Piqueras, J., García-Mesa, Y., Cárcaba, L., Feito, J., Torres-Parejo, I., Martín-Biedma, B., Cobo, J., García-Suárez, O., & Vega, J. A. (2019). Ageing of the somatosensory system at the periphery: Age-related changes in cutaneous mechanoreceptors. Journal of Anatomy, 234(6), 839–852. https://doi.org/10.1111/joa.12983
Giulio, I. D., Reeves, N. D., Roys, M., Buckley, J. G., Jones, D. A., Gavin, J. P., Baltzopoulos, V., & Maganaris, C. N. (2020). Stair gait in older adults worsens with smaller step treads and when transitioning between level and stair walking. Frontiers in Sports and Active Living, 2, 63. https://doi.org/10.3389/fspor.2020.00063
Gross, A. L., Xue, Q. L., Bandeen-Roche, K., Fried, L. P., Varadhan, R., McAdams-DeMarco, M. A., Walston, J., & Carlson, M. C. (2016). Declines and impairment in executive function predict onset of physical frailty. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 71(12), 1624–1630. https://doi.org/10.1093/gerona/glw067
Harada, E. T, & Suto, S. (2006). How cognitive aging affects the relationship between attention and error repetitions. Proceedings of the Annual Meeting of the Cognitive Science Society, 28. https://escholarship.org/uc/item/5223h5j2
Herman, T., Mirelman, A., Giladi, N., Schweiger, A., & Hausdorff, J. M. (2010). Executive control deficits as a prodrome to falls in healthy older adults: A prospective study linking thinking, walking, and falling. The Journals of Gerontology. Series A, Biological sciences and medical sciences, 65(10), 1086–1092. https://doi.org/10.1093/gerona/glq077
Hignett, S., & Wolf, L. (2016). Reducing inpatient falls: Human factors & ergonomics offers a novel solution by designing safety from the patients’ perspective. International Journal of Nursing Studies, 59, A1–A3. https://doi.org/10.1016/j.ijnurstu.2016.02.007
Hoogendam, Y. Y., van der Lijn, F., Vernooij, M. W., Hofman, A., Niessen, W. J., van der Lugt, A., Ikram, M. A., & van der Geest, J. N. (2014). Older age relates to worsening of fine motor skills: A population-based study of middle-aged and elderly persons. Frontiers in Aging Neuroscience, 6, 259. https://doi.org/10.3389/fnagi.2014.00259
Hunter, S. K., Pereira, H. M., & Keenan, K. G. (2016). The aging neuromuscular system and motor performance. Journal of Applied Physiology, 121(4), 982–995. https://doi.org/10.1152/japplphysiol.00475.2016
Kattenstroth, J. C., Kolankowska, I., Kalisch, T., & Dinse, H. R. (2010). Superior sensory, motor, and cognitive performance in elderly individuals with multi-year dancing activities. Frontiers in Aging Neuroscience, 2, 31. https://doi.org/10.3389/fnagi.2010.00031
Kearney, F. C., Harwood, R. H., Gladman, J. R., Lincoln, N., & Masud, T. (2013). The relationship between executive function and falls and gait abnormalities in older adults: A systematic review. Dementia and Geriatric Cognitive Disorders, 36(1-2), 20–35. https://doi.org/10.1159/000350031
Klimova, B., Valis, M., & Kuca, K. (2017). Cognitive decline in normal aging and its prevention: A review on non-pharmacological lifestyle strategies. Clinical Interventions in Aging, 12, 903–910. https://doi.org/10.2147/CIA.S132963
Kolev, V., Falkenstein, M., & Yordanova, J. (2005). Aging and error processing: Time-frequency analysis of error-related potentials. Journal of Psychophysiology, 19(4), 289-297. https://doi.org/10.1027/0269-8803.19.4.289
Kyllonen, P. C., & Zu, J. (2016). Use of response time for measuring cognitive ability. Journal of Intelligence, 4(4), 14.
Liu, C.-j., Shiroy, D. M., Jones, L. Y., & Clark, D. O. (2014). Systematic review of functional training on muscle strength, physical functioning, and activities of daily living in older adults. European Review of Aging and Physical Activity, 11(2), 95-106. https://doi.org/10.1007/s11556-014-0144-1
Logue, R., Goldenkoff, E., Vesia, M., & Brown, S. (2020). Measuring hand function in older adults: The need for better assessment tools. Innovation in Aging, 4(Supplement 1), 202. https://doi.org/10.1093/geroni/igaa057.653
Manard, M., Carabin, D., Jaspar, M., & Collette, F. (2014). Age-related decline in cognitive control: The role of fluid intelligence and processing speed. BMC Neuroscience, 15(1), 7. https://doi.org/10.1186/1471-2202-15-7
Mirelman, A., Herman, T., Brozgol, M., Dorfman, M., Sprecher, E., Schweiger, A., Giladi, N., & Hausdorff, J. M. (2012a). Executive function and falls in older adults: New findings from a five-year prospective study link fall risk to cognition. PLOS One, 7(6), e40297. https://doi.org/10.1371/journal.pone.0040297
Mirelman, A., Herman, T., Brozgol, M., Dorfman, M., Sprecher, E., Schweiger, A., Giladi, N., & Hausdorff, J. M. (2012b). Executive function and falls in older adults: New findings from a five-year prospective study link fall risk to cognition. PLOS One, 7(6), e40297. https://doi.org/10.1371/journal.pone.0040297
Nouchi, R., & Kawashima, R. (2014). Improving cognitive function from children to old age: A systematic review of recent smart ageing intervention studies. Advances in Neuroscience, 2014, 235479. https://doi.org/10.1155/2014/235479
World Health Organization. (2008). WHO global report on falls prevention in older age. World Health Organization.
World Health Organization. (2021). Falls. https://www.who.int/news-room/fact-sheets/detail/falls
Pothisiri, W., Prasitsiriphon, O., & Aekplakorn, W. (2020). Extent of aging across education and income subgroups in Thailand: Application of a characteristic-based age approach. PLOS One, 15(12), e0243081. https://doi.org/10.1371/journal.pone.0243081
Pothisiri, W., & Quashie, N. T. (2018). Preparations for old age and well-being in later life in Thailand: Gender matters?. Journal of Applied Gerontology, 37(6), 783–810. https://doi.org/10.1177/0733464816649281
Reve, E. v. h., & Bruin, E. D. d. (2014). Strength-balance supplemented with computerized cognitive training to improve dual task gait and divided attention in older adults: A multicenter randomized-controlled trial.BMC Geriatrics, 14(1), 134. https://doi.org/10.1186/1471-2318-14-134
Righi, V., Sayago, S., & Blat, J. (2017). When we talk about older people in HCI, who are we talking about? towards a ‘Turn to Community’ in the design of technologies for a growing ageing population. International Journal of Human-Computer Studies, 108, 15-31. https://doi.org/10.1016/j.ijhcs.2017.06.005
Rogers, M. E., Rogers, N. L., Takeshima, N., & Islam, M. M. (2004). Reducing the risk for falls in the homes of older adults. Journal of Housing For the Elderly, 18(2), 29-39. https://doi.org/10.1300/J081v18n02_04
Rosado-Artalejo, C., Carnicero, J. A., Losa-Reyna, J., Castillo, C., Cobos-Antoranz, B., Alfaro-Acha, A., Rodríguez-Mañas, L., & García-García, F. J. (2017). Global performance of executive function is predictor of risk of frailty and disability in older adults. The Journal of Nutrition, Health & Aging, 21(9), 980–987. https://doi.org/10.1007/s12603-017-0895-2
Salthouse T. A. (1979). Adult age and the speed-accuracy trade-off. Ergonomics, 22(7), 811–821. https://doi.org/10.1080/00140137908924659
Seidler, R. D., Bernard, J. A., Burutolu, T. B., Fling, B. W., Gordon, M. T., Gwin, J. T., Kwak, Y., & Lipps, D. B. (2010). Motor control and aging: Links to age-related brain structural, functional, and biochemical effects. Neuroscience and Biobehavioral Reviews, 34(5), 721–733. https://doi.org/10.1016/j.neubiorev.2009.10.005
Selgrade, B. P., Childs, M. E., & Franz, J. R. (2020). Effects of aging and target location on reaction time and accuracy of lateral precision stepping during walking. Journal of Biomechanics, 104, 109710. https://doi.org/10.1016/j.jbiomech.2020.109710
Shafizadeh, M., Sharifnezhad, A., & Wheat, J. (2019). Age-related changes to motor synergies in multi-joint and multi-finger manipulative skills: A meta-analysis. European Journal of Applied Physiology, 119(10), 2349–2362. https://doi.org/10.1007/s00421-019-04216-4
Sitzman, D. M., Rhodes, M. G., Tauber, S. K., & Liceralde, V. R. (2015). The role of prior knowledge in error correction for younger and older adults. Aging, Neuropsychology and Cognition, 22(4), 502–516. https://doi.org/10.1080/13825585.2014.993302
Smith, G. A., & Brewer, N. (1995). Slowness and age: Speed-accuracy mechanisms. Psychology and Aging, 10(2), 238–247. https://doi.org/10.1037//0882-7974.10.2.238
Song, G.-b., & Park, E.-C. (2016). Effects of neck and trunk stabilization exercise on balance in older adults. The Journal of Korean Physical Therapy, 28(4), 221-226. https://doi.org/10.18857/jkpt.2016.28.4.221
Spedden, M. E., Malling, A. S. B., Andersen, K. K., & Jensen, B. R. (2017). Association between gross-motor and executive function depends on age and motor task complexity. Developmental Neuropsychology, 42(7-8), 495–506. https://doi.org/10.1080/87565641.2017.1399129
Starns, J. J., & Ratcliff, R. (2010). The effects of aging on the speed-accuracy compromise: Boundary optimality in the diffusion model. Psychology and Aging, 25(2), 377–390. https://doi.org/10.1037/a0018022
Vallesi, A., Tronelli, V., Lomi, F., & Pezzetta, R. (2021). Age differences in sustained attention tasks: A meta-analysis. Psychonomic Bulletin & Review, 28(6), 1755–1775. https://doi.org/10.3758/s13423-021-01908-x
Vandervoort A. A. (2002). Aging of the human neuromuscular system. Muscle & Nerve, 25(1), 17–25. https://doi.org/10.1002/mus.1215
Vandierendonck A. (2017). A comparison of methods to combine speed and accuracy measures of performance: A rejoinder on the binning procedure. Behavior Research Methods, 49(2), 653–673. https://doi.org/10.3758/s13428-016-0721-5
Viseux F. J. F. (2020). The sensory role of the sole of the foot: Review and update on clinical perspectives. Neurophysiologie Clinique, 50(1), 55–68. https://doi.org/10.1016/j.neucli.2019.12.003
Voelcker-Rehage, C. (2008). Motor-skill learning in older adults—A review of studies on age-related differences. European Review of Aging and Physical Activity, 5(1), 5-16. https://doi.org/10.1007/s11556-008-0030-9
Wickremaratchi, M. M., & Llewelyn, J. G. (2006). Effects of ageing on touch. Postgraduate Medical Journal, 82(967), 301–304. https://doi.org/10.1136/pgmj.2005.039651
Zanto, T. P., & Gazzaley, A. (2017). Selective attention and inhibitory control in the aging brain. In R. Cabeza, L. Nyberg, & D. Park (Eds.), Cognitive neuroscience of aging: linking cognitive and cerebral aging, (2nd ed., pp.207-234). Oxford University Press.