A Prototype for a Mobile Peritoneal Dialysis Unit, Case Study of Lamsonthi Model, Lopburi Province
Main Article Content
Abstract
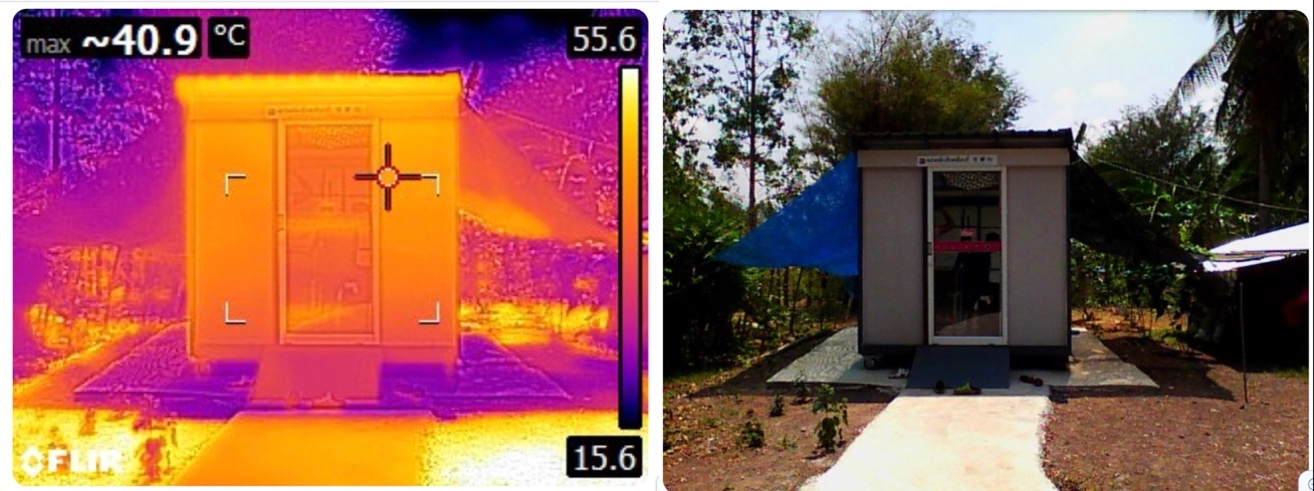
Chronic kidney disease has been a major health problem in Thailand as confirmed by the growing number of patients every year in every region. Reports pointed out that poverty and difficult access to public hospitals are among factors that prevent underprivileged kidney disease patients in rural areas from receiving proper medical treatments. Frequent visits, at least twice-a-week, to the nearest haemodialysis center are not always affordable, while many dwellings do not meet hygienic standard for home treatments. A mobile peritoneal dialysis unit invention was then initiated by Lamsonthi Hospital, Lopburi, as a part of alternative services known as “Lamsonthi Model” in attempt to fill in service gaps and transform healthcare provisions to fit specific conditions in rural villages. Researched and designed by the Built Environment for Health research unit of Kasetsart University, the prototype was developed through participatory design process between designers, patients and multidisciplinary staffs from Lamsonthi Hospital to create an integrative design outcome responsive to sensitive conditions. With emphasis on affordability and movability, the final design proposed a budget foldable prototype that can be transported in a truck and installed at any location, and later movable to another place to service another patient in need. The unit accommodates wheelchair access and is equipped with sanitary and lighting systems. The post-occupancy assessment of the prototype installed for a 25-year-old male patient at his village home since September 2016 suggested that the unit is able to support required peritoneal dialysis procedures and deal with limitations of rural home environment for the medical treatments. While the prototype still needs further development on material weight and interior environmental comfort, the invention represents a convergence through multidisciplinary approaches to transform healthcare services and encourages awareness of the necessary collaborations between medical discipline and built environment. At the same time, it demonstrates an alternative community-based approach toward specific problems in healthcare that cannot be solved by the traditional system alone.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
All material is licensed under the terms of the Creative Commons Attribution 4.0 International (CC-BY-NC-ND 4.0) License, unless otherwise stated. As such, authors are free to share, copy, and redistribute the material in any medium or format. The authors must give appropriate credit, provide a link to the license, and indicate if changes were made. The authors may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use. The authors may not use the material for commercial purposes. If the authors remix, transform, or build upon the material, they may not distribute the modified material, unless permission is obtained from JARS. Final, accepted versions of the paper may be posted on third party repositories, provided appropriate acknowledgement to the original source is clearly noted.
References
Albert, S. M. (2010). Impacts of cultural, social, and community environments on home care. in The role of human factors in home health car: workshop, Washington, DC: The National Academies Press.
Arnstein, Sherry R. (1969). A ladder of citizen participation. Journal of the American Institute of Planners, 35(4),216-224. Retrieved February 1, 2014, from http://www.tandfonline.com
Borasi, G. & Zardini, M. (Ed.) (2012) Imperfect Health. The medicalization of architecture. Canadian Center for Architecture: Montreal. Lars Müller Publishers: Zürich.
Gesler, W., Bell, M., Curtis, S., Hubbard, P., & Francis, S. (2004). Therapy by design: Evaluating the UK hospital building program. Health & Place, 10(2), 117-128.
Nissenson, A. R. & Fine, R. N. (Ed.) (2017). Handbook of Dialysis Therapy. Elsevier.
Pateman, C. (1970). Participation and Democratic Theory. Cambridge: Cambridge University Press.
Rollins, J. A. (2004). Evidence-based hospital design improves health care outcomes for patients, families, and staff. Pediatric Nursing, 30, 338- 339.
Sanoff, H. (Ed.). (2007). Special issue on participatory design. Design Studies, 28(3), 213-215.
Schneekloth, L. H. & Shibley, R. G. (2000). Implacing architecture into the practice of placemaking. Journal of Architectural Education, 53(3), 130–140.
Till, J. (2005). The negotiation of hope. In Jones PB, et al. Architecture and participation. Oxon: Spon Press.
Till, J. (2006). The architect and the other, [Online]. Retrieved January 12, 2018, from https://www.opendemocracy.net/.
Wibulpolprasert, S. (Ed.). (2008). Thailand health profile 2008-2010, [Online]. Retrieved March 26, 2018, from http://wops.moph.go.th/ops/thp/thp/en/index.php
Wilkinson, R. G. (1997). Comment: income, inequality, and social cohesion in American. Journal of Public Health, 87, 1504-1506
World Health Organization. (1948). Preamble to the constitution. Geneva, Switzerland.