中医药基于抑制病理性血管生成在肝纤维化治疗中的研究进展
คำสำคัญ:
肝纤维化, 病理性血管生成, 肝星状细胞, 抗纤维化, 中药บทคัดย่อ
肝纤维化是由于瘢痕组织在肝脏内形成所致,这一过程导致了健康肝组织的逐渐被取代。若不进行有效治疗,可能导致肝功能出现障碍,并最终演变为功能衰竭的严重后果。肝脏纤维化通常源于慢性肝病的发展,包括但不限于乙型或丙型肝炎、过度饮酒以及非酒精性脂肪肝等病因。在肝纤维化的病理过程中,病理性血管生成扮演着至关重要的角色,它通过促进肝内新血管的增生来发挥作用。这些新生血管的出现有助于减少肝脏受损区域的范围,从而诱导肝星状细胞(Hepatic stellate cells,HSCs)的激活。HSCs承担着生成过多胶原蛋白及其他细胞外基质蛋白的任务,这一过程促进了肝纤维化的进展。多项研究表明,中药可通过抑制血管内皮生长因子及血管生成素-2等促血管生成因子的产生,并减少内皮细胞增殖,表现出抗血管生成作用。中医药(Traditional Chinese medicine,TCM)治疗以病理性血管生成为靶点,为治疗肝纤维化提供了潜在选择。该综述强调了中医在治疗肝纤维化中对病理性血管生成的独特认识,可能为未来的研究提供基础。
เอกสารอ้างอิง
Affò, S.Sancho-Bru, P. CCL2: a link between hepatic inflammation, fibrosis and angiogenesis? Gut, (2014). 63(12), 1834-1835. 10.1136/gutjnl-2014-306905.
Anand, P., Kunnumakkara, A. B. Bioavailability of curcumin: problems and promises. Molecular Pharmaceutics, (2007). 4(6), 807-818.
Aschner, M., Skalny, A. V. The role of hypoxia-inducible factor 1 alpha (HIF-1α) modulation in heavy metal toxicity. Archives of Toxicology, (2023). 97(5), 1299-1318. 10.1007/s00204-023-03483-7.
Attia, A. A., Salama, A. F. Amygdalin potentiates the anti-cancer effect of Sorafenib on Ehrlich ascites carcinoma and ameliorates the associated liver damage. Scientific Reports, (2022). 12(1), 6494. 10.1038/s41598-022-10517-0.
Baghaei, K., Mazhari, S. Therapeutic potential of targeting regulatory mechanisms of hepatic stellate cell activation in liver fibrosis. Drug Discovery Today, (2022). 27(4), 1044-1061. 10.1016/j.drudis.2021.12.012.
Bernard, M., Yang, B. Autophagy drives fibroblast senescence through MTORC2 regulation. Autophagy, (2020). 16(11), 2004-2016. 10.1080/15548627.2020.1713640.
Böttcher, K.Pinzani, M. Pathophysiology of liver fibrosis and the methodological barriers to the development of anti-fibrogenic agents. Advanced Drug Delivery Reviews, (2017). 121, 3-8. 10.1016/j.addr.2017.05.016.
Gan, C., Cai, Q. Inflammasomes and Pyroptosis of Liver Cells in Liver Fibrosis. Frontiers in Immunology, (2022). 13, 896473. 10.3389/fimmu.2022.896473.
Ginès, P., Castera, L. Population screening for liver fibrosis: Toward early diagnosis and intervention for chronic liver diseases. Hepatology (Baltimore, Md.), (2022). 75(1), 219-228. 10.1002/hep.32163.
Guo, Y.-C.Lu, L.-G. Antihepatic Fibrosis Drugs in Clinical Trials. Journal of Clinical and Translational Hepatology, (2020). 8(3), 304-312. 10.14218/JCTH.2020.00023.
Higashi, T., Friedman, S. L. Hepatic stellate cells as key target in liver fibrosis. Advanced Drug Delivery Reviews, (2017). 121, 27-42. 10.1016/j.addr.2017.05.007.
Hussein, K. H., Park, K.-M. Decellularized hepatic extracellular matrix hydrogel attenuates hepatic stellate cell activation and liver fibrosis. Materials Science & Engineering. C, Materials For Biological Applications, (2020). 116, 111160. 10.1016/j.msec.2020.111160.
Kamm, D. R.McCommis, K. S. Hepatic stellate cells in physiology and pathology. The Journal of Physiology, (2022). 600(8), 1825-1837. 10.1113/JP281061.
Kisseleva, T.Brenner, D. Molecular and cellular mechanisms of liver fibrosis and its regression. Nature Reviews. Gastroenterology & Hepatology, (2021). 18(3), 151-166. 10.1038/s41575-020-00372-7.
Kityania, S., Nath, R. Acteoside (Verbascoside): A Prospective Therapeutic Alternative against Hepatocellular Carcinoma by Inhibiting the Expression of AXL, FGFR, BRAF, TIE2 and RAF1 Targets. Combinatorial Chemistry & High Throughput Screening, (2023). 26(10), 1907-1919. 10.2174/1386207326666221031121426.
Li, H. Advances in anti hepatic fibrotic therapy with Traditional Chinese Medicine herbal formula. Journal of Ethnopharmacology, (2020). 251, 112442. 10.1016/j.jep.2019.112442.
Mahmud, S., Chemaitelly, H. Characterizing trends and associations for hepatitis C virus antibody prevalence in the Middle East and North Africa: meta-regression analyses. Scientific Reports, (2022). 12(1), 20637. 10.1038/s41598-022-25086-5.
Makino, Y., Hikita, H. CTGF Mediates Tumor-Stroma Interactions between Hepatoma Cells and Hepatic Stellate Cells to Accelerate HCC Progression. Cancer Research, (2018). 78(17), 4902-4914. 10.1158/0008-5472.CAN-17-3844.
Medina, J., Arroyo, A. G. Angiogenesis in chronic inflammatory liver disease. Hepatology (Baltimore, Md.), (2004). 39(5), 1185-1195.
Neshat, S. Y., Quiroz, V. M. Liver Disease: Induction, Progression, Immunological Mechanisms, and Therapeutic Interventions. International Journal of Molecular Sciences, (2021). 22(13). 10.3390/ijms22136777.
Nobakht, M., Fattahi, M. A study on the teratogenic and cytotoxic effects of safflower extract. Journal of Ethnopharmacology, (2000). 73(3), 453-459.
Parola, M.Pinzani, M. Liver fibrosis: Pathophysiology, pathogenetic targets and clinical issues. Molecular Aspects of Medicine, (2019). 65, 37-55. 10.1016/j.mam.2018.09.002.
Petersen, J., Dandri, M. Prevention of hepatitis B virus infection in vivo by entry inhibitors derived from the large envelope protein. Nature Biotechnology, (2008). 26(3), 335-341. 10.1038/nbt1389.
Puche, J. E., Saiman, Y. Hepatic stellate cells and liver fibrosis. Comprehensive Physiology, (2013). 3(4), 1473-1492. 10.1002/cphy.c120035.
Ramos-Tovar, E.Muriel, P. Molecular Mechanisms That Link Oxidative Stress, Inflammation, and Fibrosis in the Liver. Antioxidants (Basel, Switzerland), (2020). 9(12). 10.3390/antiox9121279.
Rosmorduc, O.Housset, C. Hypoxia: a link between fibrogenesis, angiogenesis, and carcinogenesis in liver disease. Seminars In Liver Disease, (2010). 30(3), 258-270. 10.1055/s-0030-1255355.
Schwabe, R. F., Tabas, I. Mechanisms of Fibrosis Development in Nonalcoholic Steatohepatitis. Gastroenterology, (2020). 158(7), 1913-1928. 10.1053/j.gastro.2019.11.311.
Song, L., Chen, T.-Y. Pterostilbene prevents hepatocyte epithelial-mesenchymal transition in fructose-induced liver fibrosis through suppressing miR-34a/Sirt1/p53 and TGF-β1/Smads signalling. British Journal of Pharmacology, (2019). 176(11), 1619-1634. 10.1111/bph.14573.
Tong, G., Chen, X. Fibroblast growth factor 18 attenuates liver fibrosis and HSCs activation via the SMO-LATS1-YAP pathway. Pharmacological Research, (2022). 178, 106139. 10.1016/j.phrs.2022.106139.
Xiao, Z., Ji, Q. Amygdalin Ameliorates Liver Fibrosis through Inhibiting Activation of TGF-β/Smad Signaling. Chinese Journal of Integrative Medicine, (2023). 29(4), 316-324. 10.1007/s11655-021-3304-y.
Xue, X., Zhao, X. Carthami flos extract against carbon tetrachloride-induced liver fibrosis via alleviating angiogenesis in mice. Phytomedicine : International Journal of Phytotherapy and Phytopharmacology, (2023). 108, 154517. 10.1016/j.phymed.2022.154517.
ดาวน์โหลด
เผยแพร่แล้ว
รูปแบบการอ้างอิง
ฉบับ
ประเภทบทความ
สัญญาอนุญาต
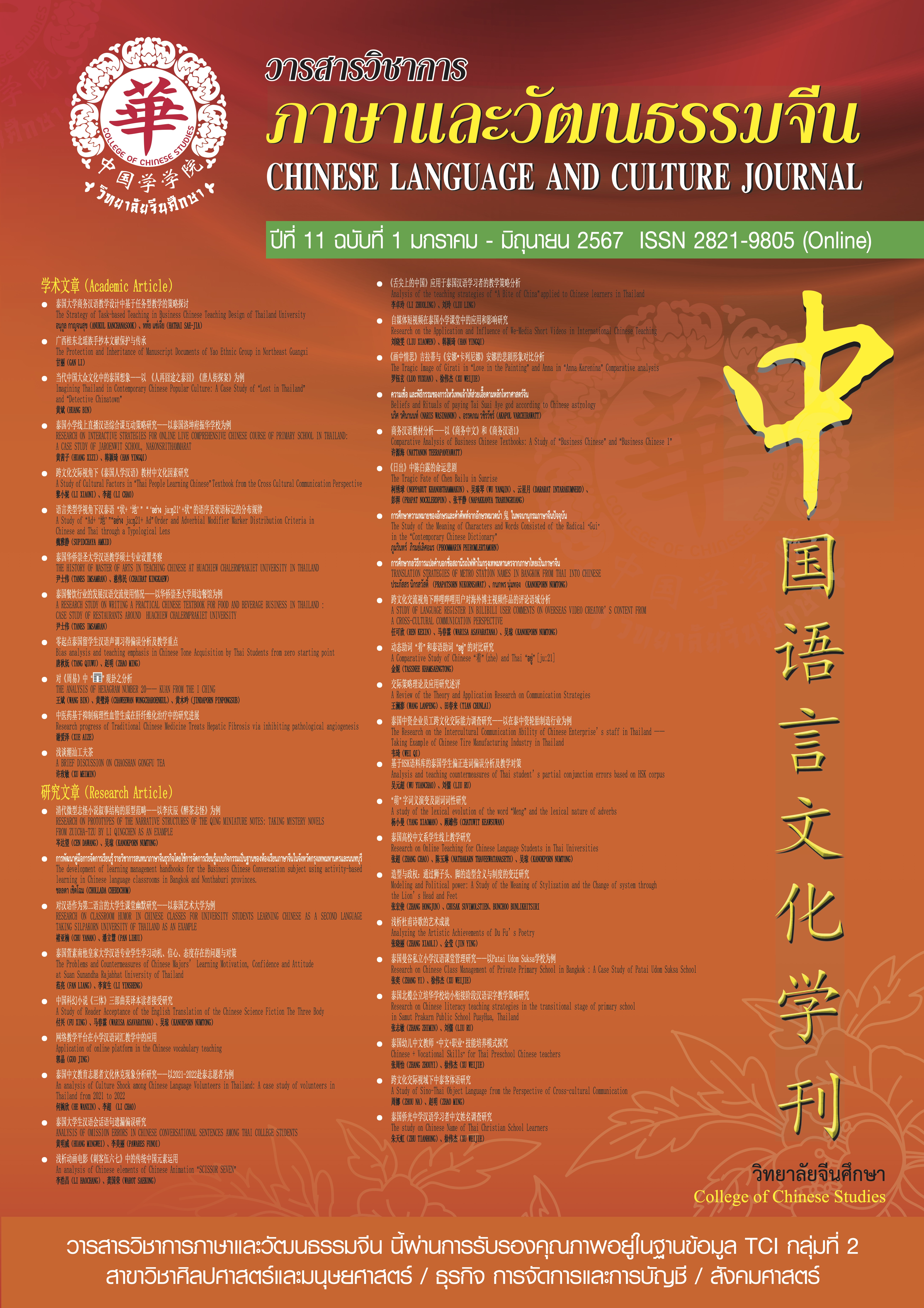
ลิขสิทธิ์ (c) 2024 วารสารวิชาการภาษาและวัฒนธรรมจีน

อนุญาตภายใต้เงื่อนไข Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
บทความที่ได้รับการตีพิมพ์เป็นลิขสิทธิ์ของวารสารภาษาและวัฒนธรรมจีน มหาวิทยาลัยหัวเฉียวเฉลิมพระเกียรติ
บทความใน “วารสารวิชาการภาษาและวัฒนธรรมจีน” เป็นทรรศนะของผู้เขียนโดยเฉพาะ กองบรรณาธิการไม่มีส่วนในความคิดเห็นในข้อเขียนเหล่านั้น